We are reporting a rare case of large substernal multinodular goiter in a 68-year-old white female. The patient had a history of goiter for more than 20 years. She complained of dyspnea, dysphagia and change of voice. Computed tomography (CT) scan of the neck and chest showed compression of the trachea and multiple pulmonary emboli. Doppler studies of the upper and lower extremities showed deep venous thrombosis (DVT) of the left brachial vein. The patient had thyroidectomy with medical therapy of pulmonary embolism.
Multinodular goiters are usually slowly growing and obstructive symptoms almost always develop insidiously [1]. Enlargement of substernal multinodular goiter may cause mechanical compression of the trachea and esophagus causing dyspnea and dysphagia, respectively. Venous congestion and thrombosis of the superior vena cava and its branches are rare. Surgical intervention in early stage is the key of treatment.

A 68 -year-old woman with a past medical history of hypertension and multinodular goiter presented to our hospital complaining of progressive shortness of breath, dysphagia and change of her voice. She denied chest pain, palpitations, wheezing, cough and hemoptysis, upper or lower extremities pain and swelling. Vital signs showed heart rate 86/min, respiratory rate 16/min, blood pressure of 148/98 mmHg and oxygen saturation of 100% on room air. Physical exam was only significant for multinodular goiter with unidentifiable inferior border of the thyroid gland.
Laboratory investigations including cardiac enzymes, arterial blood gas, basal metabolic panel, complete blood picture, B-type natriuretic peptide, coagulation profile and thyroid function tests were either normal or negative. D-dimer was elevated 1.7 mg/l.
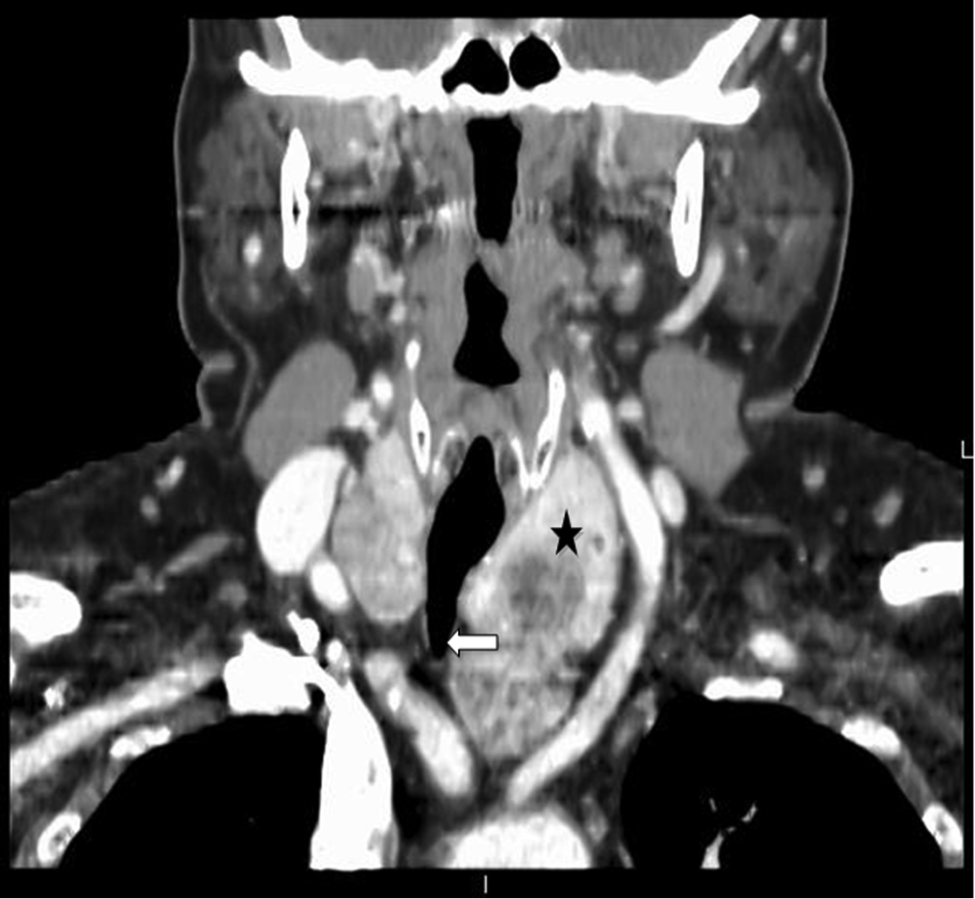
Enhanced CT scan of the neck showed asymmetrical enlargement of the thyroid gland with extension of the left thyroid lobe substernally into the mediastinum. This was accompanied by compression and flattening of the tracheal airway at the thoracic inlet with tracheal deviation to the right side (Figures 1, 2, 3). Enhanced CT scan of the chest showed multiple pulmonary emboli. Venous Doppler study of the upper and lower extremities was significant for DVT of the left brachial vein.

The patient underwent subtotal thyroidectomy using Kocher technique, followed by L-thyroxine therapy. Pulmonary embolism was treated medically with intravenous heparin. Pathological analysis of the thyroid tissue confirmed multi-nodular goiter with absence of malignancy. Three years following the surgery; she continues to be asymptomatic with no limitations.
Multinodular goiter is more common in women during the fifth and sixth decades of life [2]. It is clear that multinodular goiters are usually slowly growing and large size represents long standing disease [3]. Patients with substernal goiter may present with dyspnea, wheezes, cough or dysphagia as a result of airway or esophageal compression [4] [5] [6]. Neural and venous compression can lead to hoarseness of voice, venous thrombosis or superior vena cava syndrome [7]. Exertional dyspnea is the most common manifestation of substernal goiter that represents 30-60% of the cases [8]. Approximately 25% of patients with large cervical multinodular goiter have either subclinical hyperthyroidism, or less commonly, overt hyperthyroidism [9].
Initial evaluation of substernal goiter includes thyroid function tests to evaluate possible concomitant hyperthyroidism [6]. CT scan or magnetic resonance imaging (MRI) of the neck and chest should be conducted to evaluate the extent of the goiter and its effect on the surrounding structures [6] [10]. Chest X- ray is less sensitive than CT and MRI and may show superior mediastinal narrowing. Esophageal compression can be assessed by endoscopic ultrasonography which can distinguish between extrinsic compression and submucosal tumor with 95% to 100% accuracy [11].
Medical treatment is usually unsuccessful in such patients and surgical intervention is recommended [4]. Surgery is indicated in patients with symptoms of compression onto adjacent structures such as the trachea, esophagus and the superior vena cava. Asymptomatic patients with substernal goiter should also be considered for surgery to prevent complications [12]. These patients may present with rapid deterioration and airway obstruction as a result of superimposed infection or haemorrahge into the mediastinal component of the retrosternal goiter. Several surgical approaches have been suggested including cervical incision, sternotomy, thoracotomy and combined approaches [13].
Substernal goiter is more often benign; but it can be malignant in 2-22% of patients [7]. Mediastinal extension of substernal goiter may be life threatening as a result of airway compression, superior vena cava obstruction or pulmonary embolism. Dyspnea occurs when more than 70% of the tracheal diameter decreases [6]. Other causes are decompensated right-sided heart failure and pleural effusion [14]. Although deep venous thrombosis of the upper extremities, as a complication of substernal goiter, had been reported; pulmonary embolism was never previously reported. To our knowledge, this is the first documented case for substernal multinodular goiter complicated with pulmonary embolism as a complication of DVT of the upper extremities.
- Jauregui R, Lilker E, Bayley A. Upper airway obstruction in euthyroid goiter. JAMA. 1977;238:2163-6 pubmed
- Katlic M, Wang C, Grillo H. Substernal goiter. Ann Thorac Surg. 1985;39:391-9 pubmed
- Torre G, Borgonovo G, Amato A, Arezzo A, Ansaldo G, De Negri A, et al. Surgical management of substernal goiter: analysis of 237 patients. Am Surg. 1995;61:826-31 pubmed
- Tsang F, Wan I, Lee T, Ng S, Yim A. Management of retrosternal goitre with superior vena cava obstruction. Heart Lung Circ. 2007;16:312-4 pubmed
- Madjar S, Weissberg D. Retrosternal goiter. Chest. 1995;108:78-82 pubmed
- Jameson JL, Weetman AP. Disorders of The Thyroid Gland, In: Jameson JL, editor. Harrison’s Endocrinology, McGraw-Hill; 2013. p. 89-90.
- Tsakiridis K, Visouli A, Zarogoulidis P, Karapantzos E, Mpakas A, Machairiotis N, et al. Resection of a giant bilateral retrovascular intrathoracic goiter causing severe upper airway obstruction, 2 years after subtotal thyroidectomy: a case report and review of the literature. J Thorac Dis. 2012;4:41-8 pubmed publisher
- Rieu M, Bekka S, Sambor B, Berrod J, Fombeur J. Prevalence of subclinical hyperthyroidism and relationship between thyroid hormonal status and thyroid ultrasonographic parameters in patients with non-toxic nodular goitre. Clin Endocrinol (Oxf). 1993;39:67-71 pubmed
- Jennings A. Evaluation of substernal goiters using computed tomography and MR imaging. Endocrinol Metab Clin North Am. 2001;30:401-14, ix pubmed
- Hwang J, Saunders M, Rulyak S, Shaw S, Nietsch H, Kimmey M. A prospective study comparing endoscopy and EUS in the evaluation of GI subepithelial masses. Gastrointest Endosc. 2005;62:202-8 pubmed
- MacK E. Management of patients with substernal goiters. Surg Clin North Am. 1995;75:377-94 pubmed
- Rios A, Rodriguez J, Canteras M, Galindo P, Tebar F, Parrilla P. Surgical management of multinodular goiter with compression symptoms. Arch Surg. 2005;140:49-53 pubmed
- Anders H. Compression syndromes caused by substernal goitres. Postgrad Med J. 1998;74:327-9 pubmed
